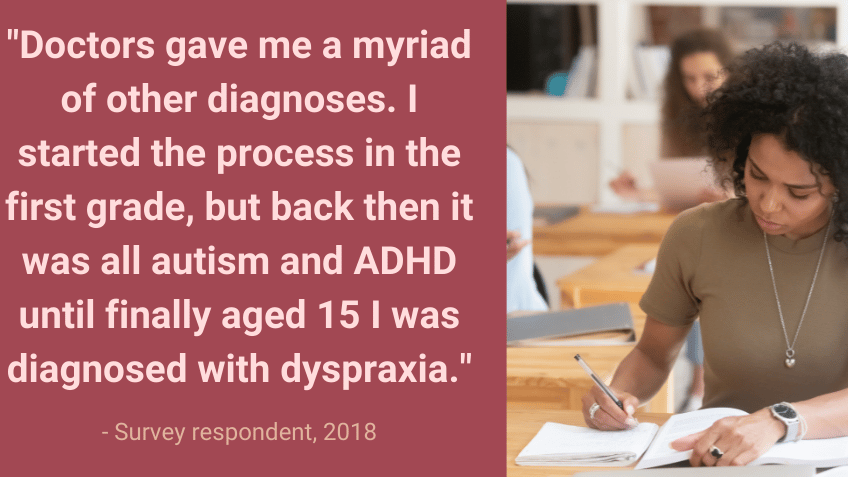
Most mental health services, guidance, and studies are geared towards the neurotypical mind – but around 1 in 10 people think differently. Neurodevelopmental conditions (NDCs) such as ADHD, autism, dyslexia, dyspraxia, learning disability and Tourette Syndrome influence how people think, perceive the world, and interact with others. These labels are helpful for providing support, understanding, and community, but real-life brains don’t always neatly fit the boxes we’ve created for them, and most people with NDCs meet the criteria for more than one.
Why do so many young people with NDCs face mental ill-health?
Co-occurring mental health conditions are also the norm rather than the exception – in part because our world was not built with the needs of neurodivergent people in mind. Despite this, people with NDCs routinely face additional barriers to getting the mental health support they need. Many have difficulty picking up on symptoms of mental ill-health as distinct from neurodivergence or communicating to other people that something is wrong. Even once they do, this often goes unrecognised by services; time and time again, we hear about children and young people being turned away by Child and Adolescent Mental Health Services because “we don’t deal with ADHD” or “autistic children are naturally more anxious, there’s nothing we can do”.
NDCs are not mental health conditions – they’re a part of who a person is and cannot be “cured” – but that doesn’t mean this group should be left without support when co-occurring mental health conditions do arise.
Yet too often, people with NDCs are punted between different pathways, each assuming that some other service will support this group because they aren’t commissioned or equipped to do so. Then, those who manage to overcome all of the above hurdles often find that the support available doesn’t work as well as it should – because people with NDCs are often excluded from research as “complicating the data”, we know too little about how effective existing mental health treatments really are outside of neurotypical people.
Thinking differently about co-occurring conditions
Too often, people with NDCs fall through the cracks in existing systems, and that’s why we set up Embracing Complexity. Embracing Complexity is a coalition of over 60 member organisations (including the Children and Young People’s Mental Health Coalition) working towards a world where everyone with NDCs can achieve their potential. We believe we can reach that goal more effectively by working together and actively focusing on the needs of people with multiple conditions. Since Embracing Complexity’s launch in 2019, we’ve called attention to how diagnostic services have restructured to pick up more than one condition at a time, highlighted the diversity of experiences of the COVID-19 pandemic and lockdown restrictions amongst people with NDCs, and set up a Special Interest Research Group exploring mental health in children and young people with NDCs.
My time working on Embracing Complexity has made clear that professionals, researchers and the community alike are keen to address the huge gaps in support for people with NDCs. Right now, mental ill-health is accepted as normal for this group – but it doesn’t have to be this way.
Author: Georgia Harper
About the author:

Georgia Harper works in the policy team at Autistica, the UK’s autism research charity, and leads the day-to-day running of Embracing Complexity. Georgia is autistic herself, and passionate about neurodivergent people leading the conversation about their own lives. Embracing Complexity is a coalition of over 60 neurodevelopmental charities and related organisations, working towards a world where everyone with neurodevelopmental conditions can achieve their potential via a more joined-up approach to diagnosis, services and research.